Overview
The Health Plan is a managed care organization, serving nearly 25,000 members. With a view to enhancing the member experience and ensuring compliance, the Health Plan decided to streamline its document-intensive appeals & grievances process.
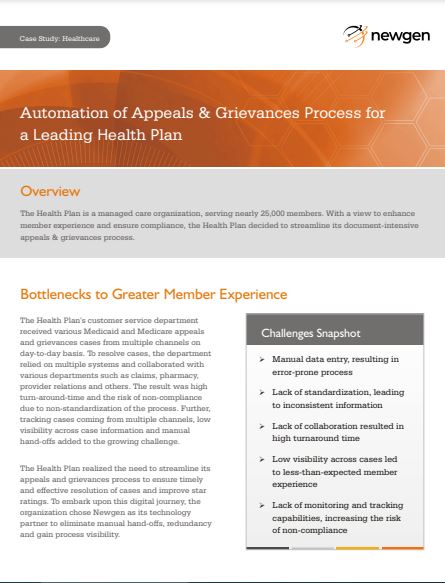
Bottlenecks to Greater Member Experience
The Health Plan’s customer service department received various Medicaid and Medicare appeals and grievances cases from multiple channels on a day-to-day basis. To resolve cases, the department relied on multiple systems and collaborated with various departments such as claims, pharmacy, provider relations, and others. The result was high turn-around-time and the risk of non-compliance due to the non-standardization of the process. Further, tracking of cases coming from multiple channels, low visibility across case information, and manual hand-offs added to the growing challenge.
The Health Plan realized the need to streamline its appeals and grievances process to ensure timely and effective resolution of cases and improve star ratings. To embark upon this digital journey, the organization chose Newgen as its technology partner to eliminate manual hand-offs, redundancy and gain process visibility.
Implementation Impact
Partnering with Newgen, the organization gained operational efficiencies and expedited its resolution process. With end-to-end visibility and easy tracking of cases, the company improved its overall member satisfaction. Further, extensive audit logs and reporting enabled the Health Plan to ensure compliance.
The Vice President of Member Services & Appeals and Grievances department summarizes his experience,
“The implementation of Newgen’s solution for streamlining complaints, appeals & grievances management has allowed for greater efficiencies in workflow management and significantly improved our Health Plan’s case integrity from a regulatory perspective. The Newgen team is an extremely dedicated partner and we are enthusiastic about our collaboration with them.”