Provider credentialing is a critical aspect of provider lifecycle management that directly impacts payer revenue, network integrity, audit performance, and patient trust.
However, in practice, credentialing is often where things slow down.
According to Medwave, the average credentialing process still takes between 90-150 days, a timeline heavily burdened by manual tasks, siloed systems, fragmented data, and endless back-and-forth communication. But, this isn’t just an operational delay. It clearly indicates that providers are left waiting to deliver care, members face longer wait time for appointments, and payers struggle with delayed claims and revenue. In short, the entire ecosystem gets adversely impacted.
As healthcare payers scale operations, expand telehealth programs, and face severe compliance scrutiny, the disjointed credentialing management systems cannot be trusted. That’s precisely why forward-looking payers are investing in modern credentialing software solutions that expedite the onboarding process, provide end-to-end visibility, and automate provider credentialing verification, all while ensuring adherence with the regulatory mandates.
However, the pressing challenge that continues to persist is: How to Choose the Best Provider Credentialing Software. In this blog, we lay down a roadmap to selecting the right credentialing management software, enabling you to introduce structure, speed, and scalability into your system.
What is Provider Credentialing?
Provider credentialing (also known as physician credentialing or medical credentialing) is a regulated process of assessing the qualifications of specific healthcare providers. This important safety check requires providers, including doctors, dentists, and other allied healthcare professionals to show they have the proper education, training and licenses to care for patients. Hospitals and health plans verify the information submitted by the provider before they are included as an in-network provider.
This process is mandated by Centers for Medicare & Medicaid Services (CMS) and the Joint Commission, with CMS requiring it to ensure only eligible providers are reimbursed for treating Medicare and Medicaid patients. Therefore, credentialing protects:
- Patients – by ensuring safe, qualified care
- Payers – by reducing chances of fraud
- Providers – by streamlining onboarding and establishing trust
Why Modern Credentialing Demands More Than Just Automation
Credentialing used to be about paperwork. Now, it’s about keeping up with the growing networks, constantly shifting regulatory mandates, and the pressure to onboard providers faster than ever. While most payers have already moved past manual workflows. The next challenge is choosing smarter systems that goes beyond automation, help teams stay compliant, avoid delays, and adapt to dynamically changing regulations.
The basics are no longer enough. Most credentialing platforms can handle standard tasks, verifications, document uploads, rosters, and applications. But, that’s just the framework. What really matters now is how well these systems support real workflows, such as reducing turnaround time, breaking down silos, adhering to the regulatory compliances, and helping teams respond quickly when regulations or provider volumes shift.
Must-have Capabilities to Look for in an Ideal Provider Credentialing Software
If automation was step one, integration, intelligence, and adaptability are what comes next. The question now isn’t whether your software can verify licenses, it’s whether it can keep the entire credentialing process connected, transparent, and scalable. Here’s what you must look for.
1. Automated Credentialing Verification
Manually verifying licenses and board certifications worked when teams were managing a handful of providers. But, with the scale most organizations are handling today, it’s just not sustainable. A smart credentialing software should plug into data sources like CAQH, DEA, and state boards so checks happen automatically, without chasing paperwork or spreadsheets.
Why it matters: Reduces manual work, errors, and ensures you’re always audit-ready.
2. Robust Document Management
It’s easy to lose track of files when they’re scattered across inboxes or shared drives. Providers should be able to upload what’s needed without back-and-forth, and your team should be able to retrieve it quickly without second-guessing if it’s the latest version.
Why it Matters: Speeds up onboarding, simplifies audits, and keeps everything organized in a unified system.
3. Dynamic Compliance Monitoring
Credentialing doesn’t stop once a provider is onboarded. Licenses expire, requirements change, and small things can slip through. That’s why your system should aways stay on top, catch early signs of red flags that doesn’t align with what NCQA and CMS guidelines.
Why it Matters: Keeps you up-to-date and eliminates surprises during audits.
4. Real-time Application Tracking
One of the biggest slowdowns in credentialing? No one has a clear view of what’s moving forward or what’s stuck. Your system must keep everyone in the loop, from internal teams managing approvals to providers waiting for updates.
Why it Matters: Improves transparency, builds trust, and saves time for constant follow-ups.
5. Built-in Communication Tools
Credentialing requires coordination. Your software should automate outreach for missing documents, track provider responses, and log everything in one place.
Why it Matters: No room for miscommunication, just smooth, trackable workflows.
6. Smart Analytics & Reporting
Your existing system might not show where delays happen. The right platform offers dashboards that track KPIs, highlight bottlenecks, and surface insights that help you work smarter.
Why it Matters: Turns credentialing from a black box into a process you can improve.
7. Roster Automation
Struggling with messy spreadsheets is no longer feasible. Simplify unstructured provider rosters into clean, standardized data inputs that sync into downstream systems like provider data management.
Read our Blog – Roster Automation-Not Just an Upgrade-Complete Transformation or Provider Onboarding.
Why it Matters: Ensures accurate data across systems and eliminates redundant entry points.
8. Enterprise-grade Security & Access Controls
Credentialing involves sensitive data. The right provider credential software must be HIPAA-compliant and include role-based access, data encryption, and audit logging.
Why it Matters: Keeps data secure and IT teams away from risk.
9. Scalability and Low-code Flexibility
Credentialing needs keep evolving. Your system should scale easily, adapt to new regulations, and support new workflows, ideally with low-code configurability.
Why it Matters: Future-proofs your operations without needing to replace the system.
10. Self-service Provider Portal
Your providers shouldn’t have to chase for updates or rely on emails for every small change. A modern portal should provide them a clean, intuitive interface to upload documents, track their credentialing progress, and respond to requests, on their own time.
Why it Matters: Improves provider experience, reduces dependency on admin teams, and keeps the process moving without friction.
11. AI-powered Process Intelligence
Choosing an AI-first solution helps flag anomalies, auto-categorize documents, predict delays, and suggest actions, all in real time.
Why it Matters: Adds intelligence to operations, enabling teams to be proactive.
Read here to learn more about why finding the perfect provider credentialing system is crucial to your health plan’s operational success.
Benefits of Provider Credentialing Software
Choosing a modern and intelligent credentialing software offers a wide array of operational advantages for healthcare payer, such as:
1. Speed Up Provider Onboarding
Eliminates long delays by automating credential verification and application processes. Faster onboarding means faster service availability for members.
2. Reduce Errors and Manual Work
Automates verifications including, licenses, certifications, and multiple documents, reducing human error and compliance risk.
3. Boost Compliance and Data Accuracy
Helps stay up to date with ever-changing NCQA, CMS, and state-level requirements through real-time integrations and low-code adaptability.
What Makes Newgen’s Provider Credentialing Management Software a Unique Choice for Health Payers?
Powered by NewgenONE, an AI-first, low-code platform, Newgen’s Provider Credentialing & Configuration Solution is built to deliver speed, compliance, and scalability across the credentialing lifecycle. Recognized by Gartner as a Representative Vendor for end-to-end provider lifecycle management, the solution brings together a robust set of capabilities that delivers transformed member experience and ensure compliance adherence.
Key Features of NewgenONE Provider Credentialing Management Software:
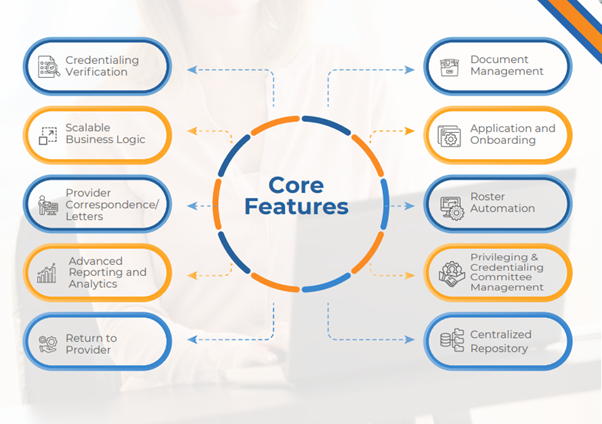
Newgen offers a complete solution tailored for health payers, designed to automate, integrate, and elevate every part of the credentialing journey.
Learn more about how Newgen Simplifies Provider Lifecycle Management Workflows for Healthcare Payers and Providers.
SCHEDULE A DEMO
You might be interested in

22 Jan, 2026
Why storing everything is not the optimal email archiving strategy for 2026



