370 % ROI
Achieved by Newgen customers
Enhance Customer Experience
by personalizing each interaction and automating the entire customer journey
15 Billion
Documents digitized in a single deployment
Automate End-to-End at Scale
by automating enterprise-wide applications while empowering a hybrid workforce
25 Patents
Powering a high performance platform
Innovate Continuously with Intelligence
by leveraging insights to optimize decisions and processes and discover new opportunities
370 % ROI
Achieved by Newgen customers
Enhance Customer Experience
by personalizing each interaction and automating the entire customer journey
15 Billion
Documents digitized in a single deployment
Automate End-to-End at Scale
by automating enterprise-wide applications while empowering a hybrid workforce
25 Patents
Powering a high performance platform
Innovate Continuously with Intelligence
by leveraging insights to optimize decisions and processes and discover new opportunities
Join Leading Global Brands










Join Leading Global Brands













Join Leading Global Brands







Join Leading Global Brands







Join Leading Global Brands











Join Leading Global Brands











Join Leading Global Brands







Join Leading Global Brands









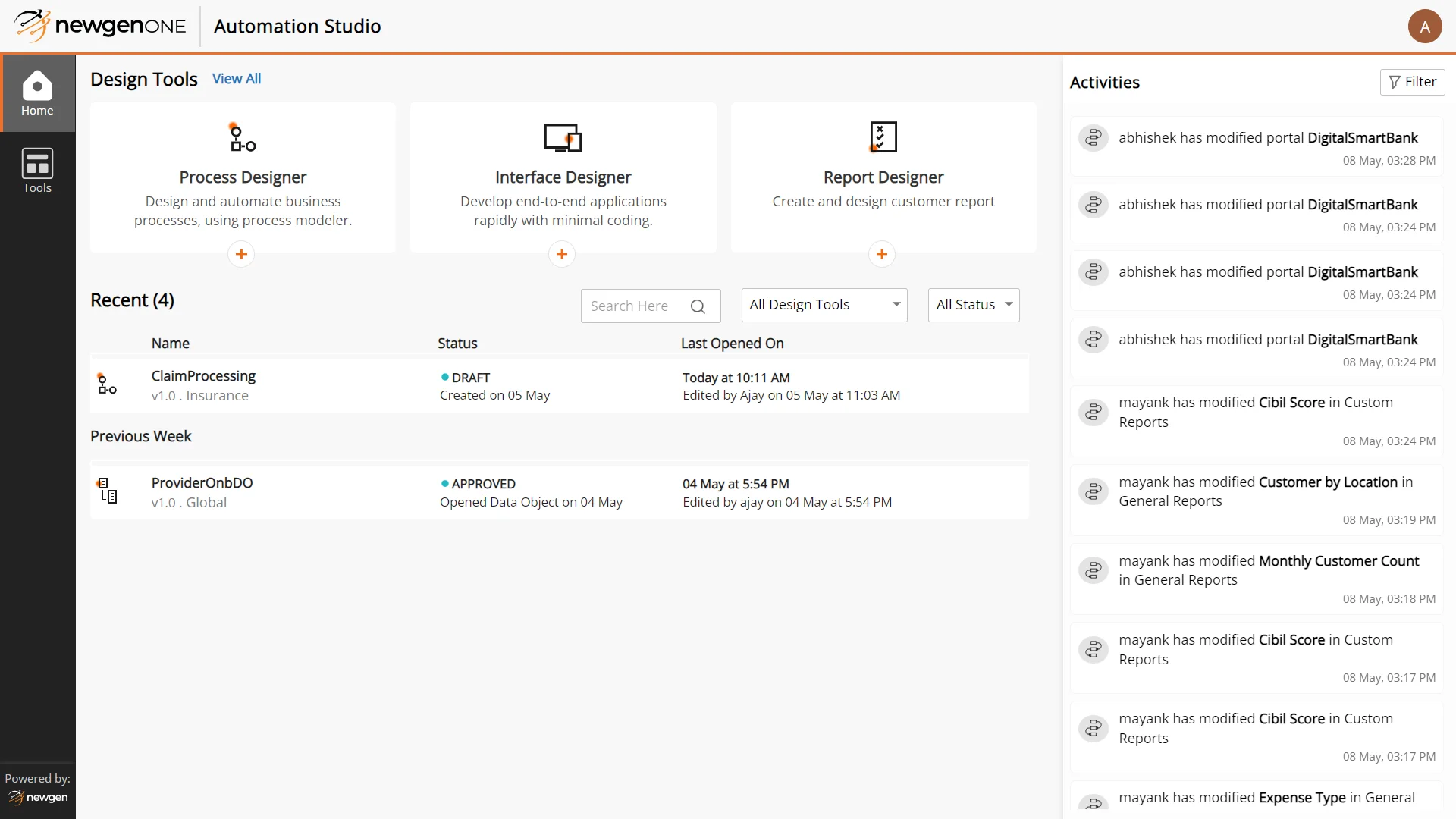
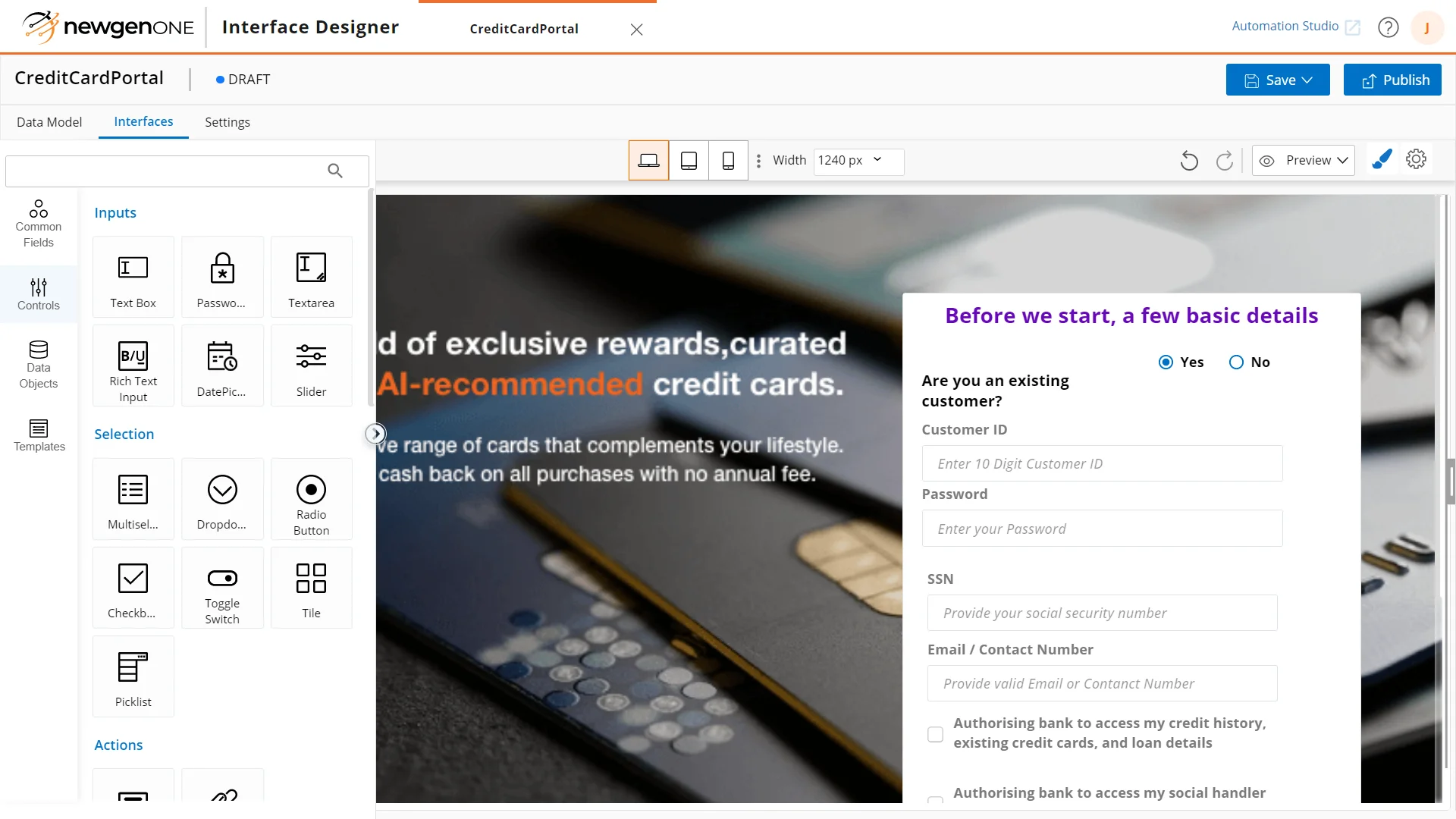
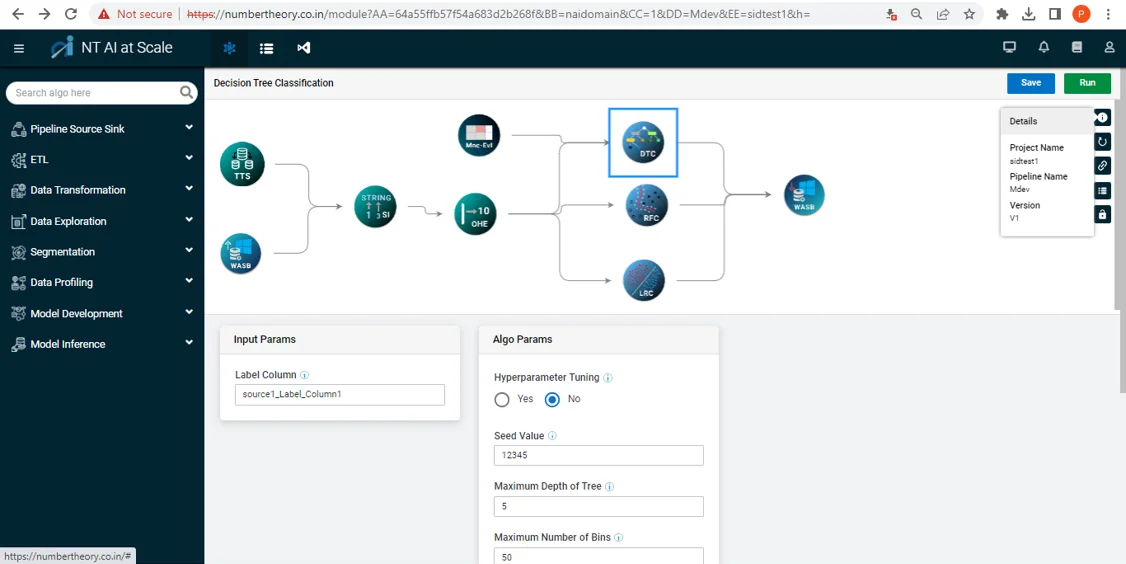
Discover NewgenONE Capabilities
Low code platform for end-to-end automation at scale
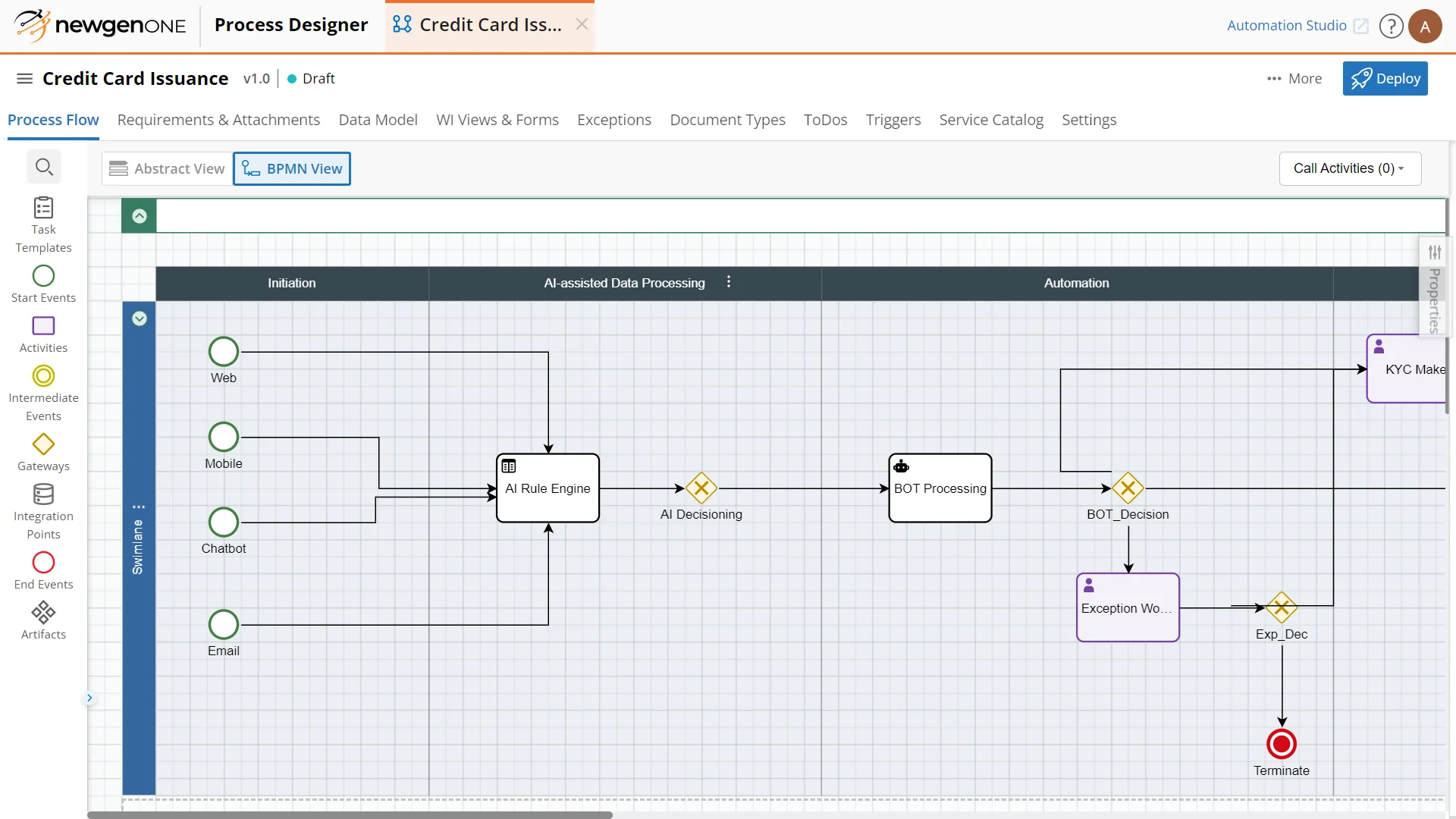
Rapidly automate end-to-end customer journeys
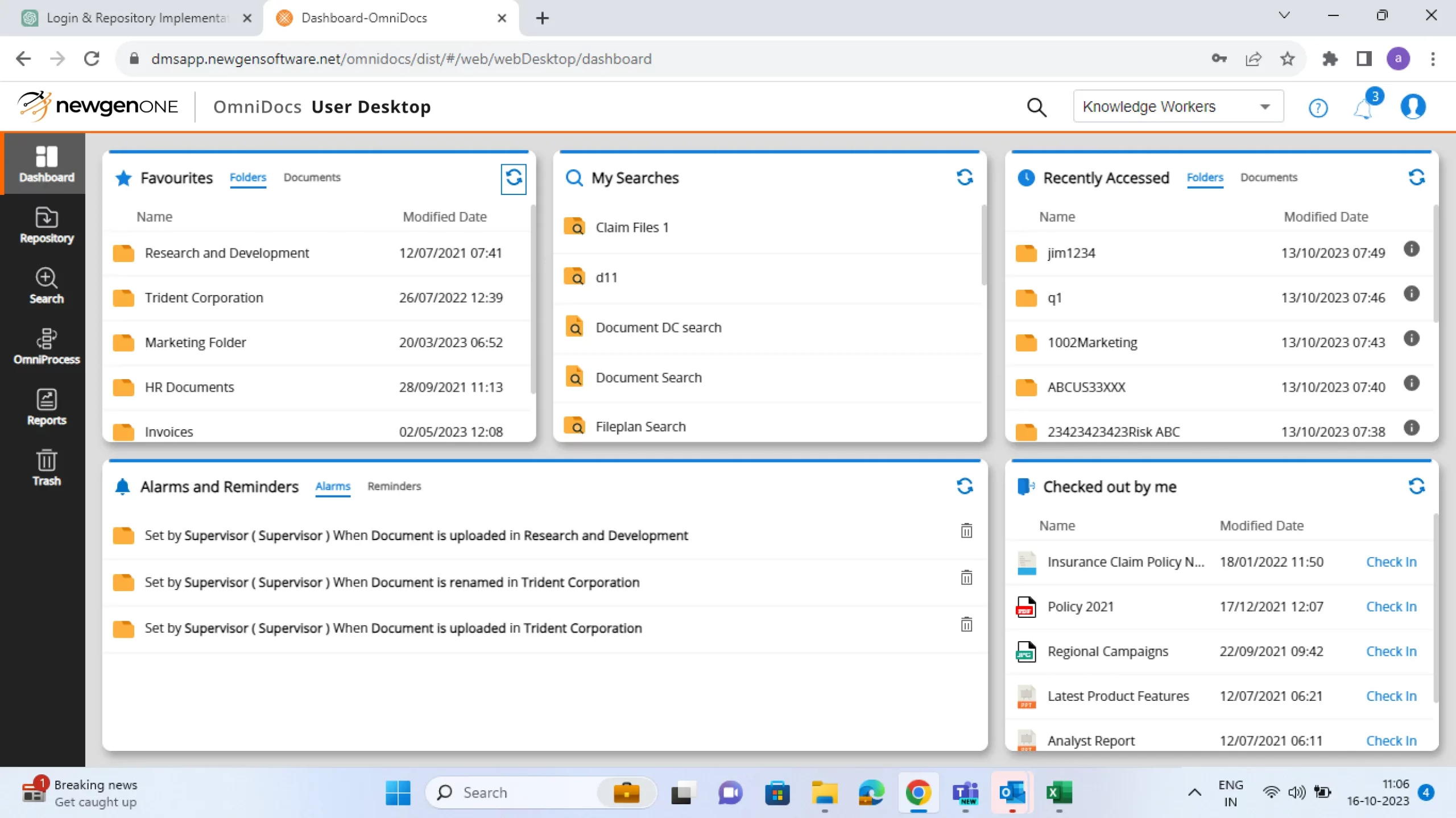
Manage content lifecycle. Ensure anytime anywhere access to content
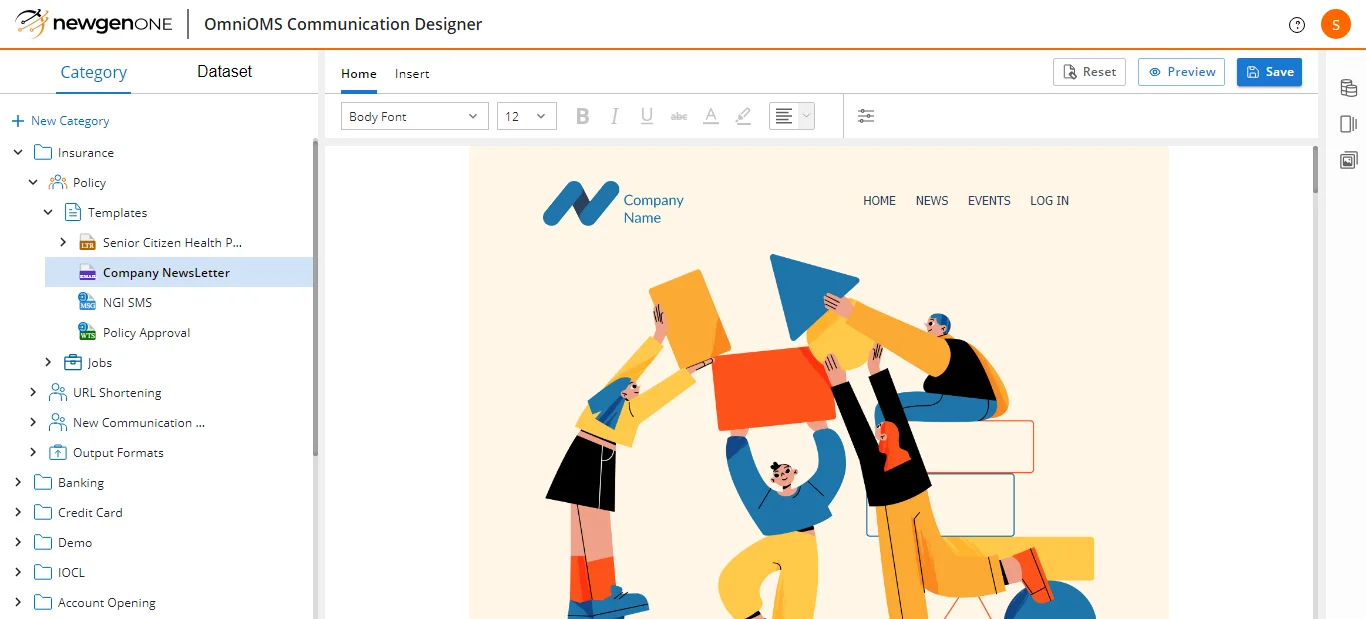
Drive real-time personalized engagement across touchpoints
Compose enterprise-grade applications at speed and scale
Make informed business decisions. Deliver transformed experience
Ready to Accelerate Digital?
See Newgen’s low-code digital transformation platform in action. Request a demo of Newgen’s platform and industry-specific applications.